Penile Implant Surgery
Am I a candidate?
A penile implant (penile prosthesis) is typically considered for men with moderate to severe erectile dysfunction (ED)who want a reliable, long-term solution—especially when other treatments have been unsuccessful or are not suitable. The goal of penile implant surgery is to restore dependable erections for sexual activity, with a device placed entirely inside the body.
You may be a good candidate if:
You have persistent erectile dysfunction that has not improved with tablets (PDE5 inhibitors), or tablets are not appropriate for you.
Injection therapy and/or a vacuum erection device (VED) have been ineffective, not tolerated, or not preferred.
You want a more spontaneous and dependable option compared with “on-demand” treatments.
ED is related to underlying medical conditions such as diabetes, vascular disease, or long-standing erectile dysfunction.
ED has occurred after prostate/pelvic surgery or pelvic treatments and has not responded to conservative therapies.
You have ED alongside penile curvature (Peyronie’s disease) where an implant may help restore function (in selected cases).
Penile implants are not usually first-line treatment
Most men will try less invasive options first. A penile implant is commonly considered when ED is significant, ongoing, and affecting quality of life, and when you’re looking for the most reliable outcome.
What your specialist will assess before surgery
A urology and andrology specialist consultation typically reviews:
Your ED history (severity, duration, response to prior treatments)
Medical conditions and medications that may affect erections or surgical risk
Any penile curvature, pain, or prior genital/pelvic surgery
Your expectations (including appearance, sensation, and likely outcomes)
Which implant type is most appropriate (inflatable vs malleable)
When an implant may need to be delayed or reconsidered
In some situations, surgery may be postponed until certain risks are optimised—such as active infection, poorly controlled medical conditions, or other factors your surgeon identifies during assessment.
If you’re unsure whether a penile implant is right for you, a consultation can clarify your options and the next best step—including whether tablets, injections, or other treatments are more appropriate before considering surgery.
What is a penile implant?
A penile implant (penile prosthesis) is a surgically implanted medical device used to treat erectile dysfunction (ED)when other treatments (tablets, injections, vacuum devices) are ineffective or unsuitable. Implants are placed entirely inside the body and allow a man to have a reliable erection for sexual activity.
There are two main types of penile implants:
Malleable (semi-rigid) implant
Three-piece inflatable implant
Types of penile implant:
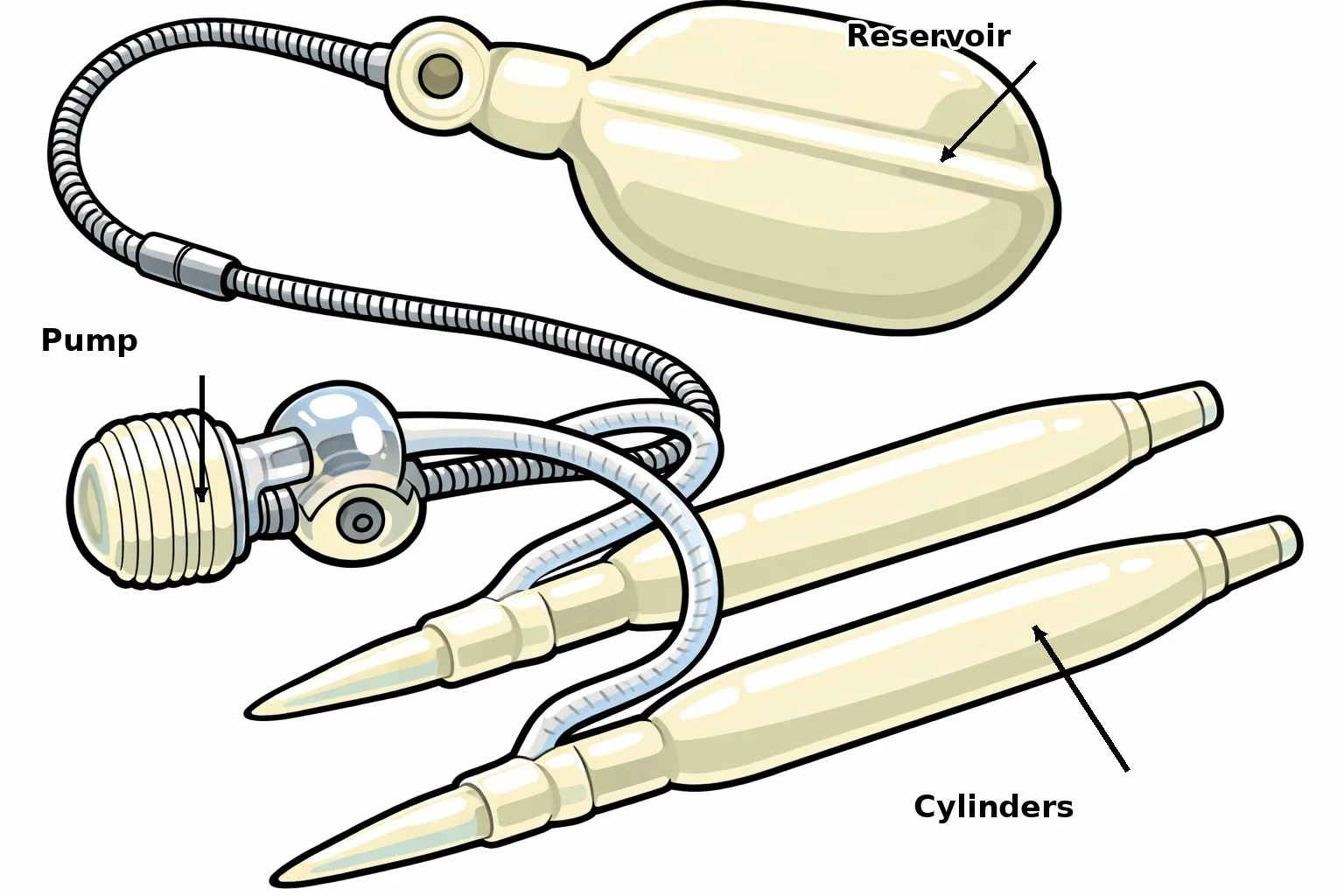
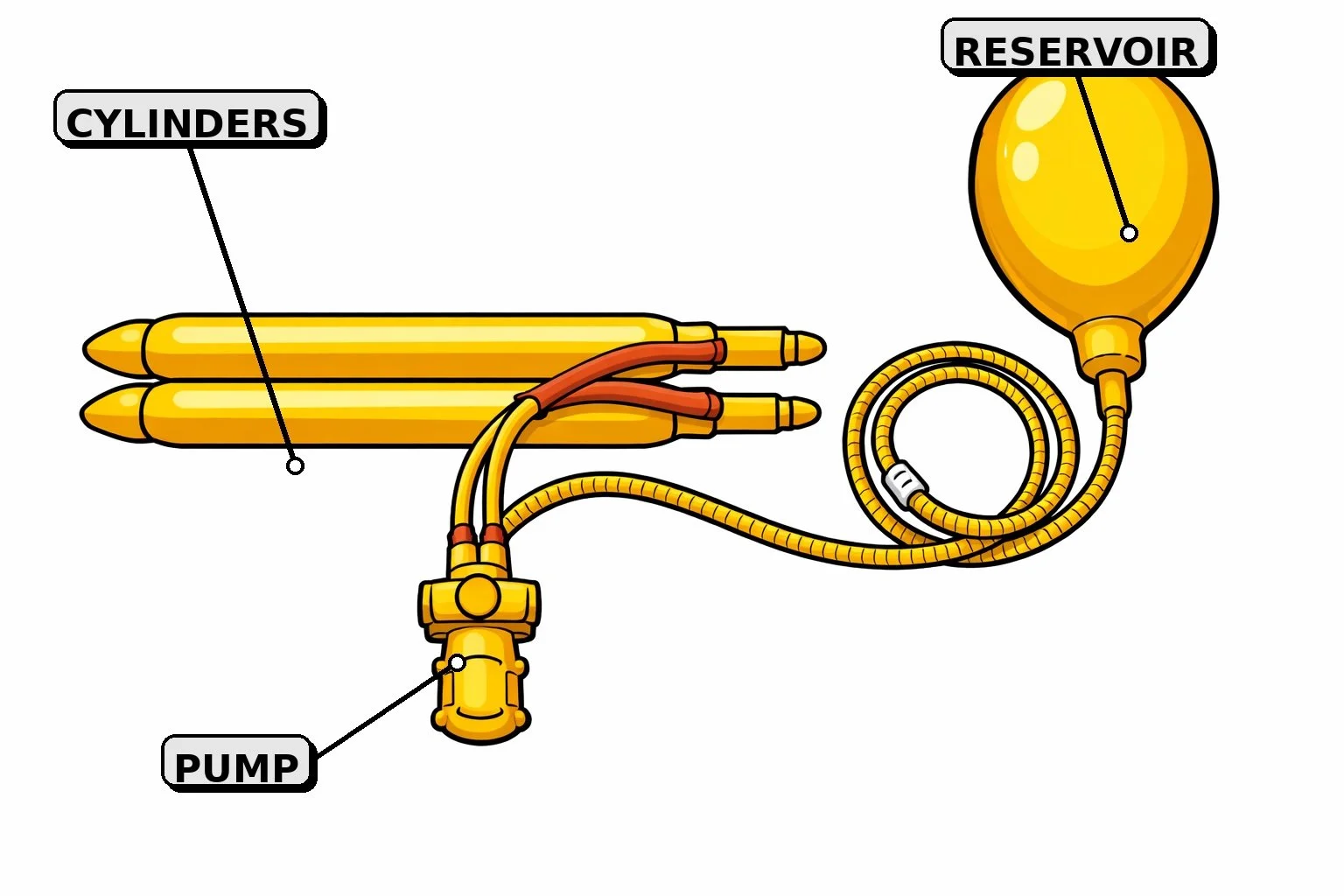
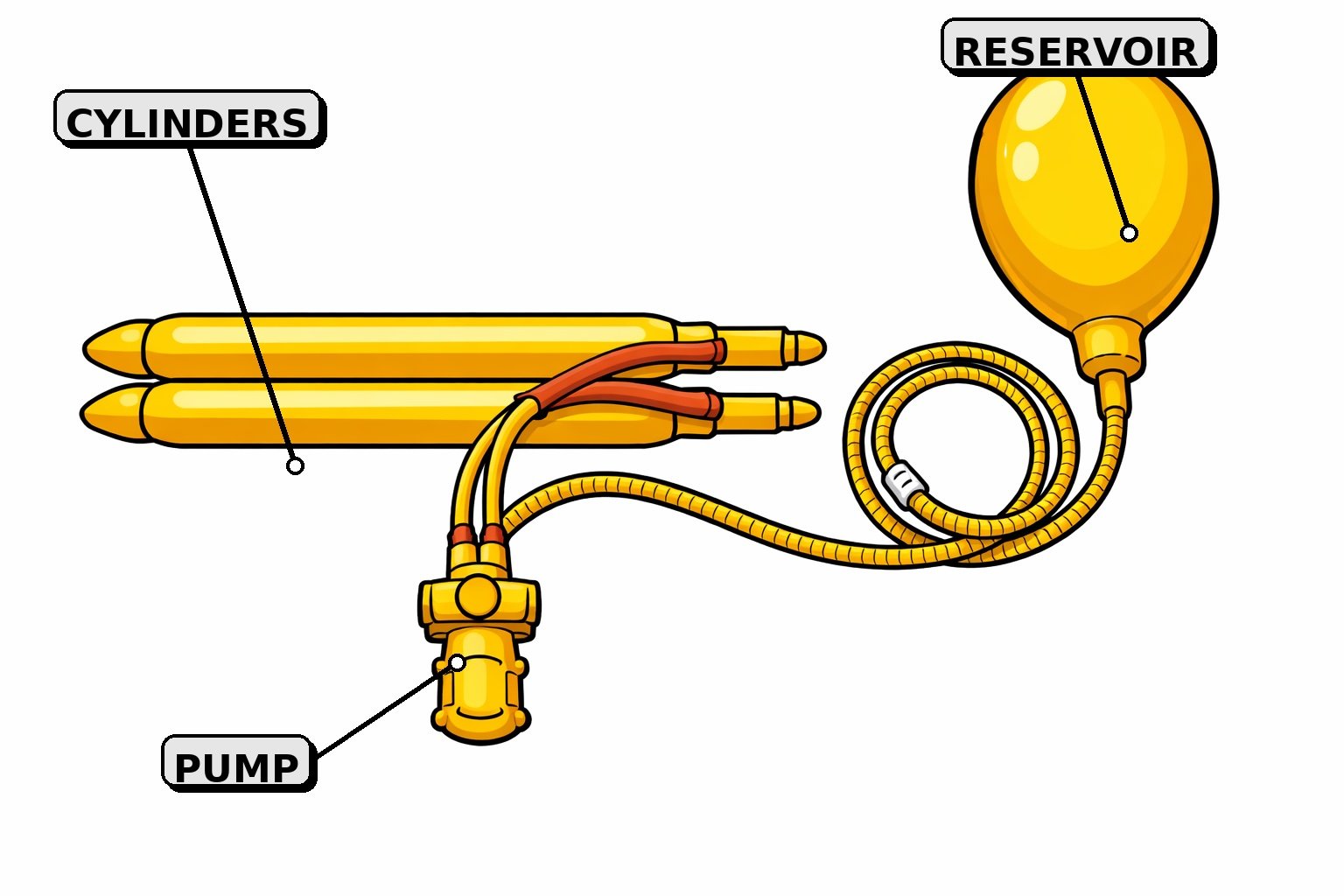
Three-Piece Inflatable Penile Implant
What is it?
A three-piece implant consists of:
Two inflatable cylinders in the penis
A fluid reservoir placed in the lower abdomen
A pump placed in the scrotum
Squeezing the pump transfers fluid into the cylinders to create an erection. Pressing the release valve returns the penis to a flaccid state.
Advantages (Pros)
Most natural look and feel
Penis is soft when deflated, firm when inflated
Best cosmetic and functional result
High patient and partner satisfaction rates
Easier to conceal under clothing
Disadvantages (Cons)
More complex surgery
Slightly higher risk of mechanical failure over time
Requires good hand function to operate the pump
Higher cost than malleable implants
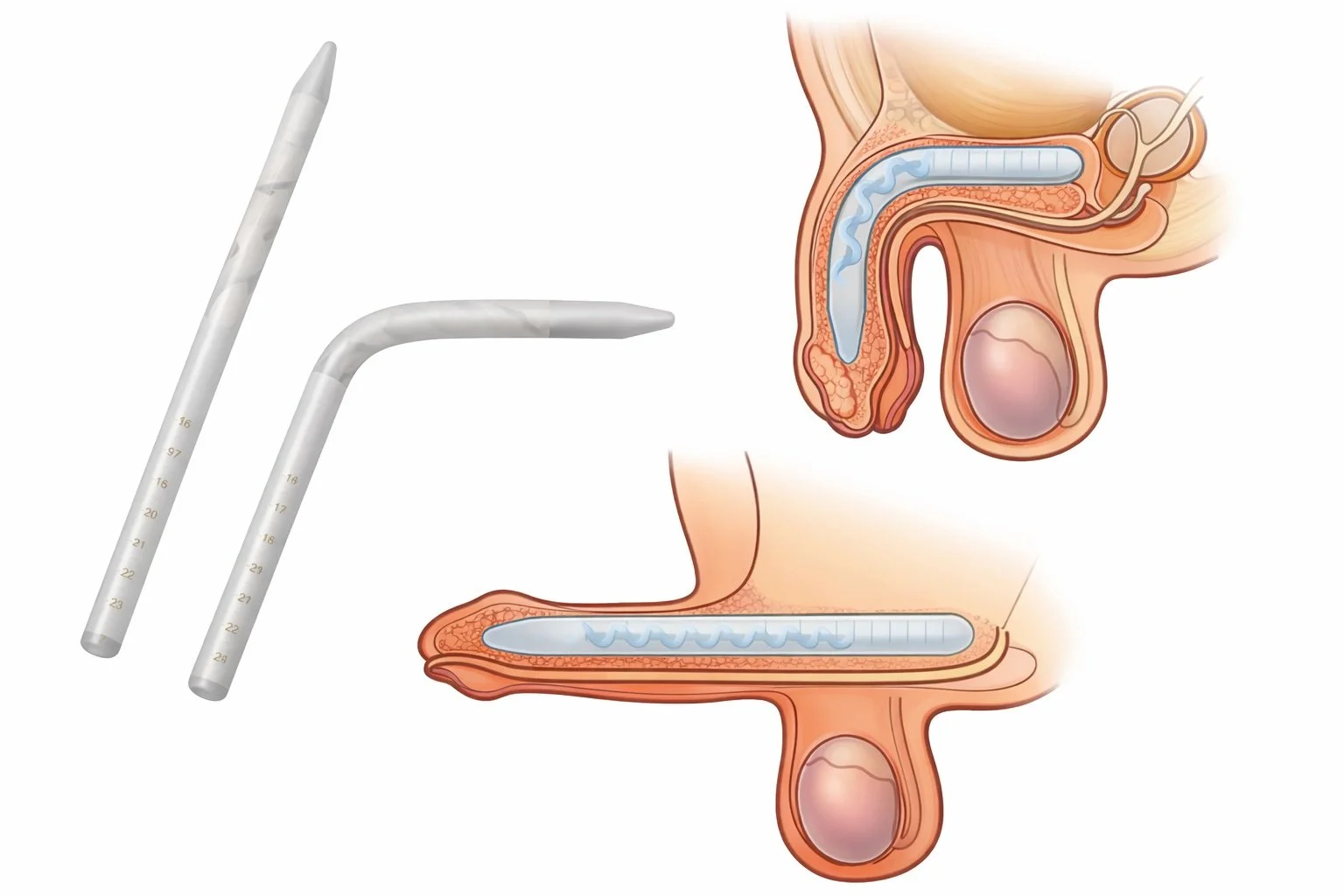
Malleable Penile Implant
What is it?
A malleable implant consists of two bendable rods placed inside the erectile chambers (corpora cavernosa) of the penis.
The penis is manually positioned up for intercourse and down for daily activities.
Advantages (Pros)
Simple design with fewer mechanical parts
Very reliable – lowest risk of mechanical failure
Easier surgery with shorter operating time
Lower cost than inflatable implants
Good option for:
Men with limited hand dexterity
Complex medical conditions
Previous infections or multiple surgeries
Disadvantages (Cons)
Penis is always semi-firm, not fully flaccid
Can be more noticeable under clothing
Less natural appearance compared to inflatable implants

Results and Expectations
This section explains what research and major urology patient resources report about penile implant surgery (penile prosthesis)—including likely outcomes, what changes (and what doesn’t), satisfaction, device longevity, and common reasons men feel disappointed. It is general information and not a substitute for personalised medical advice.
What a penile implant is designed to do
A penile implant is a surgical treatment for erectile dysfunction (ED) that restores the mechanical ability to achieve an erection firm enough for sex, on demand. Penile implants are usually considered when tablets, injections, or vacuum devices are ineffective or not suitable (this “stepwise” approach is reflected in major ED guidance).
What results most men can expect
Reliability is the main benefit
Across many studies, penile prostheses are consistently described as a highly effective option for refractory ED with high satisfaction. Reviews commonly report patient satisfaction around ~80–90%, though measurement tools vary. Wiley Online Library+3PMC+3PubMed+3
Partner satisfaction
Partner satisfaction is also generally high but can be more variable, with published ranges in some reviews spanning ~50–90% (often influenced by expectations, relationship factors, and baseline function). PubMed+1
What this means for patients: the implant is most likely to help if the primary goal is dependable erections, and expectations about size/feel are realistic.
What the implant will NOT do (common misconceptions)
It does not increase libido (sex drive)
Penile implants restore rigidity, but they do not increase sexual desire.
It does not “make you bigger”
Penile implants do not increase penis size. Some men perceive the erect penis as shorter than remembered, especially if ED has been long-standing or if there is scarring (e.g., Peyronie’s disease).
Sensation, orgasm, and ejaculation: what evidence suggests
For many men, penile implant surgery does not change skin sensation and does not prevent orgasm or ejaculation—provided those functions were present before surgery and there is no separate condition affecting them.
However, it’s important to know:
If orgasm/ejaculation/sensation were affected by prior pelvic cancer treatment, nerve injury, or another condition, an implant cannot “repair” that damage—it mainly restores erections.
Some men need time to adjust to the new sensation of the device and the mechanics of use.
What your penis will look like (inflatable vs malleable)
Inflatable (usually 3-piece) implant
Typically provides the most natural change between flaccid and erect states.
Erection is achieved by pumping fluid into the cylinders.
Malleable (semi-rigid) implant
The penis remains firm but can be positioned up or down.
Simpler mechanics, different cosmetic “resting” appearance.
(Your surgeon will recommend an option based on anatomy, goals, and medical factors.)
Device longevity: how long implants last
No implant lasts forever, but modern devices generally have strong long-term performance.
A large meta-analysis of inflatable penile prostheses reported approximate device survival of:
~87% at 5 years
~77% at 10 years
~64% at 15 years (with further decline over time) ScienceDirect
What this means for patients: many men will not need revision for a long time, but revision or replacement may eventually be required due to mechanical wear or other issues.
Risks that most influence results and how common they are
Infection
Infection is the complication patients worry about most. Contemporary reviews note that primary penile prosthesis infection rates are commonly ≤5%, and in many modern series are lower—particularly with coated devices and strict infection prevention protocols. PMC+2PMC+2
Revision surgery carries a higher infection risk than first-time implants.
Mechanical problems / revision surgery
Because implants are mechanical devices, malfunction can occur over time and may require revision or replacement. Long-term survival data above helps quantify this risk.
Penile length dissatisfaction
A frequent reason for dissatisfaction reported in reviews is perceived penile shortening, which is why expectation-setting is a major part of the consultation.
(Your surgeon will discuss your individual risk profile.)
When you can expect to see the result
Most men need a period of healing and familiarisation:
Early swelling and discomfort are common initially.
You’ll usually receive training on device use once healing is adequate.
Sexual activity resumes only after surgeon clearance.
Patient resources commonly note it may take weeks to adjust to the sensation and use.
Who gets the best outcomes
Outcomes tend to be best when:
ED is clearly defined and treatments have been tried appropriately
expectations are realistic (especially about size and what implants can/can’t change)
both patient (and partner, if applicable) understand the recovery process and device use
Key takeaways
Penile implants are an effective, durable option for severe ED, with high satisfaction commonly reported (~80–90%).
They restore erections, but do not increase libido or penis size.
They usually do not prevent orgasm or ejaculation, unless those functions are already affected by another condition.
Device survival is strong at 5–10 years, with some men needing revision over longer timeframes.
Preparation for surgery
In the weeks before
Medical optimisation matters: good diabetes control and stopping smoking reduce infection risk. You will be asked to have a urine test (to ensure sterile urine) and a MRSA screen.
Tell your surgeon if you’ve had prior pelvic surgery (e.g. prostate surgery) or hernia repair, or if you’ve had Peyronie’s disease/priapism/previous penile surgery, as this can change operative planning
Medications: your team will advise what to do with blood thinners/antiplatelets and supplements
The night before/morning of
Fasting: follow your fasting instructions (typically nil by mouth for 6 hrs prior to surgery)
Avoid shaving the genital area at home
Day of surgery
You will be admitted, meet your anaesthetist and nursing team, and have final checks.
What happens during the surgery
Previously selected penile prosthesis (malleable or 3-piece) will be sized and implanted
An indwelling urinary catheter is inserted and this is usually removed on postoperative day 1
To reduce bruising/haematoma, your surgeon will place a small suction drain and wrap the penis/scrotum in a crepe bandage
Expected inpatient stay
Most patients go home 1-2 days after surgery (this varies with surgeon preference, your medical history, and how you recover)
The catheter is removed the morning after surgery
Before discharge you should be:
comfortable on oral pain relief
passing urine
walking safely
clear on wound care and follow-up
After care
What to expect (first few days)
Swelling and bruising of the penis/scrotum is common
Pain is common but will resolve in a few weeks
Wound care
Keep dressings as advised by your team and keep the wound clean and dry
Avoid sitting in bath/pools for 4 weeks
Can shower as normal following discharge
Activity
Supportive underwear will greatly support your comfort and recovery
Avoid heavy lifting/strenuous physical activity for 6 weeks following surgery
You are to avoid all forms of sexual activity for 6 weeks after surgery
Using the device
A follow up appointment will be scheduled at 3-4 weeks to provide training on device cycling

When to seek urgent help
Contact your surgeon or go to Emergency if you have:
fevers/chills or feel unwell
increasing redness, heat, worsening pain, pus or bad-smelling discharge from the wound
rapidly increasing swelling/tense scrotum
inability to pass urine after catheter removal
bleeding or severe pain not controlled with prescribed medication

Risks and Complications
All surgery has risks. The list below summarises the possible risks and complications of penile implant (penile prosthesis) surgery in a patient-friendly way. Your individual risk depends on your health, prior surgery, and implant type.
Common early (short-term) risks
Pain and discomfort - especially in the first days to weeks
Swelling and bruising of the penis/scrotum
Bleeding / haematoma - a collection of blood that may increase swelling and pain
Wound issues - minor bleeding, delayed healing, scarring
Infection - can be serious—may require antibiotics and, in some cases, implant removal
Device-specific risks (implant-related)
Mechanical failure over time
Fluid leak or cylinder/pump problems
Difficulty using the pump
Device malposition
Erosion or extrusion
Injury to surrounding structures
Functional risks
These aren’t dangerous, but they affect satisfaction and should be understood:
Perceived change in penis length or girth
Changes in sensation - usually minimal, but can vary
Orgasm or ejaculation issues - often related to underlying conditions or prior pelvic/prostate surgery rather than the implant itself
Persistent curvature or Peyronie’s-related changes
Partner concerns (comfort, expectations, adjustment period)
Longer-term risks
Need for revision surgery
Chronic pain
Factors that can increase risk
Diabetes (especially if poorly controlled)
Smoking
Obesity
Immune suppression or chronic steroid use
Spinal cord injury or reduced sensation
Previous penile implant or revision surgery (revision procedures generally carry higher infection risk)
History of pelvic radiation or complex pelvic surgery
What contributes to the cost of penile implant surgery?
The total cost of penile implant surgery (penile prosthesis) can vary between patients because it is made up of several separate components. The final amount depends on the type of implant, the hospital setting, and whether you have private health insurance. A written, itemised estimate is usually provided once your assessment and surgical plan are confirmed.
Costs commonly include:
Specialist consultation fees
Initial assessment, discussion of treatment options, suitability for surgery, and implant selection.Pre-operative tests
Blood tests, urine testing, ECG or other investigations if required for medical clearance.Surgeon fees
The surgical procedure itself, including planning and follow-up care.Assistant surgeon fees
Anaesthetist fees
Fees vary based on the type of anaesthesia, procedure duration, and individual medical factors.Hospital fees
Theatre costs, nursing care, consumables, and bed/stay fees (day stay vs overnight).The implant device
Costs differ between inflatable (3-piece) implants and malleable (semi-rigid) implants, and between manufacturers/models.Post-operative medications
Pain relief and antibiotics if prescribed.Post-operative follow-up and device training
Wound checks and (for inflatable implants) education on inflation/deflation once healing is adequate.
Private health insurance and out-of-pocket expenses
If you have private health insurance, your out-of-pocket costs may include:
Your excess/co-payment for hospital admission
In some cases, a device gap, depending on your policy and the fund’s benefit for the implant
Why costs vary
The overall cost is influenced by:
Implant type (inflatable vs malleable)
Hospital setting and length of stay
Surgical complexity (e.g., prior pelvic surgery, scarring/Peyronie’s disease, revision procedures)
Individual health factors that affect operating time and post-op care