Male fertility procedures
Vasectomy
What is a vasectomy?
A vasectomy is a surgical procedure to cut and seal the tubes (vas deferens) that carry sperm from the testicles. You are NOT sterile straight away after a vasectomy. Therefore you must use an alternative contraceptive method initially. You will perform a post vasectomy semen analysis to confirm it has been successful. Once confirmed sterile, you will no longer be able to make a woman pregnant naturally. You will still ejaculate normally, but the semen will not contain sperm. To perform this procedure, two small incision in the scrotum are required to access each vas. This procedure is performed under a general anaesthetic as a day procedure.
Preparation for Surgery
Deciding on a vasectomy
A vasectomy should be considered permanent contraception
It may not always be the right decision if you feel pressured, are under significant stress or are unsure about future plans
Vasectomy reversal is not guaranteed and should not be relied upon as a backup plan
Before surgery
You will receive specific instructions:
Fasting - typically no food or drink for 6 hrs prior to surgery
Medications - You may be asked to stop certain medications such as blood-thinners prior to surgery
Transport - You cannot drive yourself home after a general anaesthetic. Arrange a responsible adult to take you home and stay with you that evening.
Work and activity planning - plan for at least 2 weeks of light activity after surgery
Supportive underwear - have firm supportive underwear available to wear for 1 month after surgery

Day of Surgery
Admission and anaesthetic
You will check in as a day patient
The team will confirm your consent, medical history and fasting status
A general anaesthetic means you will be fully asleep for the procedure
After surgery, you will wake in recovery and be monitored until it is safe to go home
The procedure
You will have two small incisions in the scrotum to access each vas deferens
The skin is closed with an absorbable suture
Going home
Most men go home the same day, once comfortable, eating/drinking and passing urine
You will need an adult escort and should rest at home for the remainder of the day
Aftercare and Recovery
In the first few days
Pain, swelling and bruising are common and mild
Ensure you wear supportive underwear to help during this period
Take simple analgesia such as paracetamol and ibuprofen
Keep the area clean and dry - you can shower but avoid soaking in baths/swimming pool for 2 weeks
Activity
Take it easy for 24-48 hrs
Avoid heavy lifting, strenuous exercise and sexual activity for 2 weeks
Return to work depends on your role
desk-based work - 1-2 days
physical work - may need 1-2 weeks
Medications
You will be provided specific advice about restarting medications that were withheld for surgery
Sex and contraception - very important
You are NOT sterile straight away after a vasectomy
Sperm can remain in the ejaculate for some time
You must use an alternative method of contraception until you have a semen test confirming you are sterile
Many men need at least 20 ejaculations and a wait of several weeks before confirming you are no longer fertile on a semen test
Testing will be arrange with the clinic around 3 months
Only stop contraception when you are told it is safe to do so based on your test results
Possible risks and complications
Bruising, swelling and pain in the scrotum are common
Wound infection
Sperm granuloma
Chronic scrotal pain - rare
Early or late recanalisation
The tubes can remain open or reconnect which can lead to pregnancy even after the procedure
This is why post vasectomy semen analysis is essential
Regret
When to Seek Medical Advice
Contact your doctor or seek urgent care if you experience:
Rapidly increasing swelling, severe pain, a very enlarged scrotum
Fever or feeling unwell
Increasing redness, warmth, pus/discharge
Persistent bleeding
Any concern that symptoms are getting worse rather than better

Vasovasostomy (Vasectomy Reversal)
What is a vasovasostomy?
A vasovasostomy (often called a vasectomy reversal) is an operation to reconnect the two ends of the vas deferens (the tubes that carry sperm) after a vasectomy. The aim is to allow sperm to return to the semen, so natural pregnancy may be possible. The procedure is performed with the aid of a surgical microscope and fine needles. In some cases the surgeon may need to perform a vasoepididymostomy if there is blockage closer to the epididymis. This is more complex and can affect success rates.
Success is often described in two ways:
Patency - sperm return to the semen
Pregnancy - natural pregnancy occurs (dependent on both partners’ fertility)
Preparation for Surgery
Before the operation
Consultation and assessment: you’ll discuss your goals, medical history, and factors that influence success (e.g., time since vasectomy, prior scrotal surgery, history of infection).
Medications: you may be asked to stop certain medications such as blood-thinners prior to surgery
Smoking/vaping: stopping (even temporarily) improves healing.
Shaving: do not shave yourself prior to surgery
Fasting: typically no food or drink for 6 hrs prior to surgery
Transport: arrange someone to drive you home and stay with you overnight as this is typically performed as a day procedure under general anaesthetic
What to bring
Firm and supportive underwear to provide scrotal support, and comfortable loose clothing.
Day of Surgery
Performed under general anaesthetic
Incisions: small incisions are made on either side of the scrotum
Microsurgery: the cut ends of the vas are identified and examined. Fluid from the testicular side may be checked to help decide the best type of reconnection.
Reconnection: the vas is rejoined with multiple very fine stitches
Duration: commonly 2–4 hours (longer if more complex)
Inpatient stay - typically performed as day procedure but overnight admission may be required in some cases
After care
First 48 hours
Rest: take it easy; gentle walking is fine.
Scrotal support: wear supportive underwear day and night for the first 4 weeks
Pain relief: typically only require simple analgesia including paracetamol and ibuprofen
Wound care
Keep the area clean and dry.
You may shower after 24–48 hours (depending on dressing advice), but avoid soaking (baths/pools) until wounds are well healed.
A small amount of bruising and swelling is common.
Activity
Avoid heavy lifting, cycling, running, or gym work for about 2 weeks (or as directed).
Avoid contact sports for longer if you still have tenderness or swelling.
Sex and ejaculation
Recommend no sex or ejaculation for 2–3 weeks
Follow-up and semen testing
Semen analysis and clinical review is arranged for 3 months after surgery
Risks
All operations carry risks. Your surgeon will discuss these with you and how they apply to your situation.
Common/expected
Pain, swelling, bruising of the scrotum
Mild wound ooze or discomfort for several days
Less common but important
Bleeding/haematoma
Wound infection
Fluid collection around the testicle (hydrocele) or persistent swelling
Chronic scrotal pain
Testicular loss due to compromised blood flow
Failure to restore sperm to the semen (no patency) or later scarring/re-blockage
Need to convert to a more complex repair (vasoepididymostomy) if a blockage is found
Fertility-related
Even if sperm return, pregnancy is not guaranteed (partner factors and sperm quality matter).

When to Seek Medical Advice
Contact your doctor or seek urgent care if you experience:
Rapidly increasing swelling, severe pain, a very enlarged scrotum
Fever or feeling unwell
Increasing redness, warmth, pus/discharge
Persistent bleeding
Any concern that symptoms are getting worse rather than better

Varicocele Embolisation
What does varicocele embolisation involve?
Varicocele embolisation is performed by an interventional radiologist using X-ray guidance to block (embolise) the vein(s) causing the varicocele.
Key points:
It is minimally invasive and usually performed under local anaesthetic
It works by blocking the draining veins, and does not affect the arteries that supply blood to the testicle
The abnormal vein is blocked using small metal coils or a liquid sclerosant (a medicine that makes the vein close)
It is typically a day procedure
Success:
Around 8 out of 10 patients (80%) have a successful outcome
Why might I be offered embolisation?
You may be referred because:
You have pain/discomfort from a varicocele (often worse with standing or exercise), and/or
The varicocele is being considered as part of an infertility assessment, where treatment may help improve sperm quality in some men
What are the alternatives?
Alternatives may include:
Observation (no treatment), especially if the varicocele is small and not causing symptoms
Microsurgical repair (microsurgical clipping/ligation of veins via a small groin incision)
Preparing for the procedure
Your team will review your history and medications and confirm your consent on the day. You can still change your mind at any time.
Before you attend, you may be asked to:
Not eat for ~6 hours beforehand (you may be allowed clear fluids such as water—follow your hospital’s instructions)
Tell staff if you have allergies or have ever had a reaction to X-ray contrast dye
Make sure your team knows if you:
Take blood thinners (e.g., warfarin, aspirin, clopidogrel, rivaroxaban, dabigatran)
Have implanted devices (e.g., pacemaker, stent, joint replacement), or a history of MRSA
What happens on the day?
Where it happens:
In a radiology procedure room (angiography suite), similar to an operating theatre but with specialised X-ray equipment
Before the procedure:
You change into a gown
A small cannula is placed in a vein in your arm
Monitoring may be attached, and sedation or pain relief can be given if needed
During the procedure:
A small puncture is made (typically neck or groin) after local anaesthetic
A thin catheter and guidewire are navigated into the testicular vein
Coils and/or sclerosant are used to block the abnormal veins, with contrast dye used to check position and completeness
The catheter is removed and pressure applied to prevent bleeding; a small dressing is placed
How long it takes:
Often 45–60 minutes, but can vary
Afterwards:
You’ll be monitored for 2–3 hours, and usually go home the same day
Will it hurt?
After the initial local anaesthetic, the procedure is usually not painful
You may feel warmth when contrast dye is injected (sometimes feels like passing urine)
A small bruise can occur at the puncture site
Risks and possible after-effects
The following risks are typical for varicocele embolisation (your individual risk may vary):
Common
Bruising at puncture site: between 1 in 2 and 1 in 10
Pain at puncture site (may worsen over a few days): between 1 in 2 and 1 in 10
Back pain for 48–72 hours: between 1 in 2 and 1 in 10
Less common
Infection at puncture site needing antibiotics/drainage: between 1 in 10 and 1 in 50
Recurrence requiring repeat embolisation or surgery: between 1 in 10 and 1 in 50
Uncommon
Damage/bleeding from punctured vein requiring surgery: between 1 in 50 and 1 in 250
Coil migration into the lung (often retrievable; if not, usually unlikely to cause long-term problems but may cause cough/mild chest pain for a few days): between 1 in 50 and 1 in 250
Failure to position coils satisfactorily needing further treatment: between 1 in 50 and 1 in 250
Other notes:
Embolisation has no significant risk of testicular atrophy (shrinkage) or hydrocele (fluid around the testicle) compared with some surgical approaches.
Aftercare: what to expect at home
Rest for the remainder of the day
Most people can resume normal activities after 24 hours
Simple pain relief (e.g., paracetamol) usually helps
The veins above the testicle can feel more prominent/tender for a few days, then gradually settle (they may not disappear completely)
If you’re prescribed antibiotics or other medicines, these will be arranged
You’ll usually be given a follow-up plan/appointment
Microsurgical Varicocele Ligation
Microsurgical varicocele ligation (also called microsurgical varicocelectomy) is an operation to treat a varicocele—enlarged veins around the testicle (similar to varicose veins). It aims to reduce scrotal discomfort and, in selected men, may improve semen parameters and fertility potential.
Preparation for surgery
Your pre-operative appointment
You may be asked about:
Symptoms (ache, heaviness, swelling)
Fertility goals and semen test results (if relevant)
Past groin surgery/hernia repairs
Medications, allergies, bleeding/bruising history
Common pre-op tests may include:
Blood tests (as required)
Urine test (sometimes)
Scrotal ultrasound (if not already done)
Semen analysis and hormones (if fertility is the main concern)
Medications
Follow your surgeon/anaesthetist’s instructions carefully. Typical guidance includes:
Blood thinners (e.g., warfarin, apixaban, rivaroxaban, clopidogrel, aspirin): do not stop on your own—your team will advise a safe plan.
Anti-inflammatories (e.g., ibuprofen, naproxen): may need to be avoided close to surgery.
Continue most regular medications with a sip of water unless told otherwise.
Fasting and anaesthetic
Microsurgical varicocele ligation is commonly done as a day procedure under general anaesthetic (sometimes with local anaesthetic for extra comfort).
You’ll be given fasting instructions (usually no food for a set period before surgery).
Tell the team if you’ve had nausea after anaesthetic before, sleep apnoea, or reflux.
What to bring and plan
Supportive underwear (briefs/compression)
Loose clothing
Arrange a responsible adult to drive you home and stay with you overnight
Plan time off work:
Desk work: often 3–7 days
Heavy lifting/manual work: often 2–4 weeks (varies)
Understanding benefits and risks
Potential benefits:
Reduced scrotal ache/heaviness
Reduced varicocele size
In selected patients: improved semen parameters over time
Possible risks/complications (uncommon but important):
Bruising, swelling, wound infection
Bleeding/haematoma
Persistent pain or discomfort
Varicocele recurrence or persistence
Hydrocele (fluid collection around the testicle)
Very rarely: injury to testicular artery affecting testicular function (risk is lowest with microsurgical technique)
Day of surgery
Arrival and preparation
You’ll check in, change into a gown, and have observations taken.
The surgeon will confirm the side (left/right/both) and mark the site.
An anaesthetist will review your medical history and discuss the anaesthetic plan.
The procedure
A small incision is usually made in the lower groin (subinguinal/inguinal area).
A microscope is used to identify and preserve important structures (testicular artery and lymphatics).
Enlarged veins are tied off (ligated) to reduce abnormal backflow.
After the operation
You may notice:
Mild groin/scrotal discomfort
A small dressing over the incision
Some swelling or bruising (often peaks in the first few days)
Most patients go home the same day once pain is controlled, you can walk safely, and you’ve passed urine.
After care
Pain control
Expect soreness for several days.
Use prescribed pain relief as directed.
Many patients do well with paracetamol/acetaminophen ± anti-inflammatories (if safe for you).
Wound care
Keep the dressing clean and dry as instructed.
You may be allowed to shower after 24–48 hours—follow your surgeon’s specific advice.
Avoid soaking in baths, pools, or spas until the wound is well healed (often ~1–2 weeks).
Scrotal support and swelling
Wear supportive underwear day and night for the first week (or as advised).
Apply ice packs (wrapped in a cloth) for 10–15 minutes at a time during the first 24–48 hours to reduce swelling.
Bruising can track into the scrotum and upper thigh—this is common and usually settles.
Activity and return to work
General guidance (your surgeon may adjust this):
Walking: encouraged from day 1
Driving: when you’re off strong pain medicines and can brake safely (often 2–5 days)
Desk work: often 3–7 days
Gym and heavy lifting: usually avoid for 2–4 weeks
Cycling: often avoid for 2–3 weeks
Sexual activity/ejaculation: often safe after 1–2 weeks when comfortable (confirm with your surgeon)
Fertility follow-up
If the surgery is for fertility:
Sperm production cycles take time; changes in semen parameters are usually assessed around 3 months, and sometimes again at 6 months.
Keep any scheduled semen analysis and follow-up appointments.
When to seek urgent medical help
Contact your surgeon or seek urgent care if you have:
Fever or chills
Increasing redness, heat, or pus from the wound
Rapidly worsening pain or swelling
A tense, enlarging scrotum/groin lump
Persistent vomiting or inability to keep fluids down
Difficulty passing urine
Severe bleeding through the dressing
Microsurgical Testicular Sperm Extraction (microTESE)
What is microTESE?
MicroTESE (microsurgical testicular sperm extraction) is a specialised surgical procedure used to retrieve sperm directly from the testicle. Any sperm found can be frozen and later used for assisted reproductive techniques such as IVF with intracytoplasmic sperm injection (ICSI).
Preparation for Surgery
Before your procedure:
You will have a viral screen prior to surgery. This must be done within 3 months of surgery so that any sperm retrieved can be safely frozen.
In addition we will check your male hormonal profile to ensure this does not require medical optimisation prior to surgery
You will be asked to sign specific consent forms for the procedure and for sperm freezing and storage.
You may be advised when to stop certain medications before surgery.
Smoking cessation is strongly recommended, as smoking reduces fertility outcomes and increases surgical risks.
You will usually be asked to fast (no food or drink) for 6 hours prior to surgery.
Day of Surgery
You will be reviewed by your urologist and anaesthetist on arrival.
MicroTESE is performed under a general or spinal anaesthetic.
The surgery is performed via a small incision in the scrotum and is assisted by a high-power operating microscope.
Any sperm found is immediately sent to the embryology laboratory for freezing.
Dissolving stitches are used and do not need to be removed.
MicroTESE is a highly specialised procedure and is only available in selected centres.
Inpatient stay
This is day procedure surgery and overnight admissions are generally not required.
Pain is usually mild to moderate and managed with simple pain relief.
You will be monitored for:
Pain or excessive swelling
Bleeding or infection
Before discharge, the team will explain how the procedure went and discuss next steps for fertility treatment.
Aftercare and Recovery at Home
After going home, you can expect:
Scrotal swelling, bruising, and discomfort for several days
You will usually be given a scrotal support (jock strap); tight supportive underwear is an alternative
Pain relief such as paracetamol or ibuprofen is usually sufficient
Activity and Work
Avoid strenuous activity and heavy lifting for 4 weeks
Most patients need 5–7 days off work (longer if your job is physical)
Avoid sexual activity for 4 weeks
Possible Risks
Failure to find sperm
Scrotal bruising or swelling
Infection or bleeding
Chronic testicular pain (uncommon)
Rarely, testicular shrinkage requiring hormone treatment

When to Seek Medical Advice
Contact your surgical team if you develop:
Increasing pain, swelling, or redness
Fever or signs of infection
Worsening bruising or bleeding
Electroejaculation
Electroejaculation (sometimes called electroejaculation sperm retrieval) is a procedure used to obtain semen/ejaculate when a man cannot ejaculate normally. It is most commonly used for men with spinal cord injury or other neurological conditions affecting ejaculation, and in selected cases of anejaculation. The sample can be used for fertility treatment, including IUI or IVF/ICSI, depending on sperm quality.
Preparation for electroejaculation
Pre-procedure assessment
Your treating team will review:
Your medical history, including any spinal cord injury level, autonomic symptoms, and previous episodes of autonomic dysreflexia
Current medications (especially blood thinners)
Any urinary tract symptoms or recurrent infections
Fertility goals and partner factors (if relevant)
You may be asked to organise:
Urine test (to exclude infection)
Blood tests if required by the hospital/day surgery unit
Semen-related planning with your fertility team (collection container, lab timing, consent forms)
Autonomic dysreflexia risk - spinal cord injury
Men with spinal cord injury at or above T6 may be at risk of autonomic dysreflexia (dangerously high blood pressure) during bladder, bowel, or rectal stimulation—including electroejaculation. Your specialist will plan strategies to reduce this risk, which may include:
Blood pressure monitoring
Preventative medication (if appropriate)
Anaesthetic planning (sedation or general anaesthetic)
Fasting and anaesthetic plan
Electroejaculation is often performed under:
General anaesthetic, or
Sedation, sometimes with local measures
You will receive fasting instructions (typically no food for a set period before the procedure). Follow these exactly for safety.
Medication guidance
Blood thinners/antiplatelets: do not stop these unless your doctor instructs you.
Blood pressure medicines: your anaesthetist will advise what to take on the morning.
Tell your team about all supplements and over-the-counter medicines.
Bowel and bladder preparation
Your team may recommend:
Emptying the bladder before the procedure
In some cases, a catheter may be used
Occasionally a bowel routine/enema is recommended to reduce rectal stool and improve comfort and access
What to bring / plan
Arrange transport home (you cannot drive after sedation/anaesthetic)
Bring any mobility aids and a list of medications
If you are working with a fertility clinic, confirm timing so the sample can be processed promptly
Day of surgery
On arrival
You’ll check in, change into a gown, and have baseline observations taken.
The team will confirm your consent and the plan for sample handling (e.g., whether it is for immediate use, freezing, or diagnostic testing).
During the procedure
You will be positioned safely (often on your side or back, depending on your needs).
A specialist device delivers gentle electrical stimulation via a rectal probe to trigger ejaculation.
The procedure is performed by an experienced clinician with close monitoring, especially if you have spinal cord injury.
Collection and sample processing
Semen is collected into sterile containers.
In some situations, semen may go backward into the bladder (retrograde ejaculation). If this is likely, the team may:
Prepare the bladder beforehand, and/or
Collect and process urine after the procedure to retrieve sperm
How long does it take?
The procedure itself is usually short, but allow several hours overall for admission, anaesthetic, recovery, and lab handling.
Recovery area
Afterwards you may experience:
Mild rectal discomfort or a sense of “fullness”
Light spotting (uncommon, usually minimal)
Temporary fatigue from anaesthetic/sedation
If you have spinal cord injury: monitoring continues for autonomic symptoms until stable
Most patients go home the same day once safe.
Aftercare and recovery
Pain and comfort
Most people have little pain afterwards.
Use simple pain relief if needed (as advised).
If you have rectal discomfort, it typically settles within 24–48 hours.
Activity
Rest on the day of the procedure.
Return to normal daily activities the next day if you feel well.
Avoid heavy exercise for 24 hours (or as advised).
Do not drive, operate machinery, or sign legal documents for 24 hours after sedation/anaesthetic.
Passing urine and hydration
Drink fluids and pass urine normally after the procedure.
A small amount of burning the first time you urinate can occur if catheterisation was used.
Seek help if you cannot pass urine.
Sexual activity
If you feel comfortable and your doctor agrees, sexual activity can usually resume within 24–48 hours.
If the procedure is part of fertility treatment, follow your fertility specialist’s timing instructions.
Fertility plan and results
Your clinic will advise what happens next, which may include:
Immediate use of the sample for IUI or IVF/ICSI
Cryopreservation (freezing) for future treatment
A report of semen parameters if this was a diagnostic procedure
Risks and possible complications
Electroejaculation is generally safe when performed by experienced teams, but risks can include:
Common or expected
Temporary rectal discomfort
Temporary fatigue from sedation/anaesthetic
Uncommon
Rectal irritation or minor bleeding
Urinary tract infection (especially if catheterisation is required)
Vasovagal symptoms (light-headedness)
Important
Autonomic dysreflexia (sudden high blood pressure, headache, flushing, sweating, anxiety). This is a medical emergency if severe and requires prompt treatment—your team will monitor for this during and after the procedure.
Seminal Vesiculography (under General Anaesthetic)
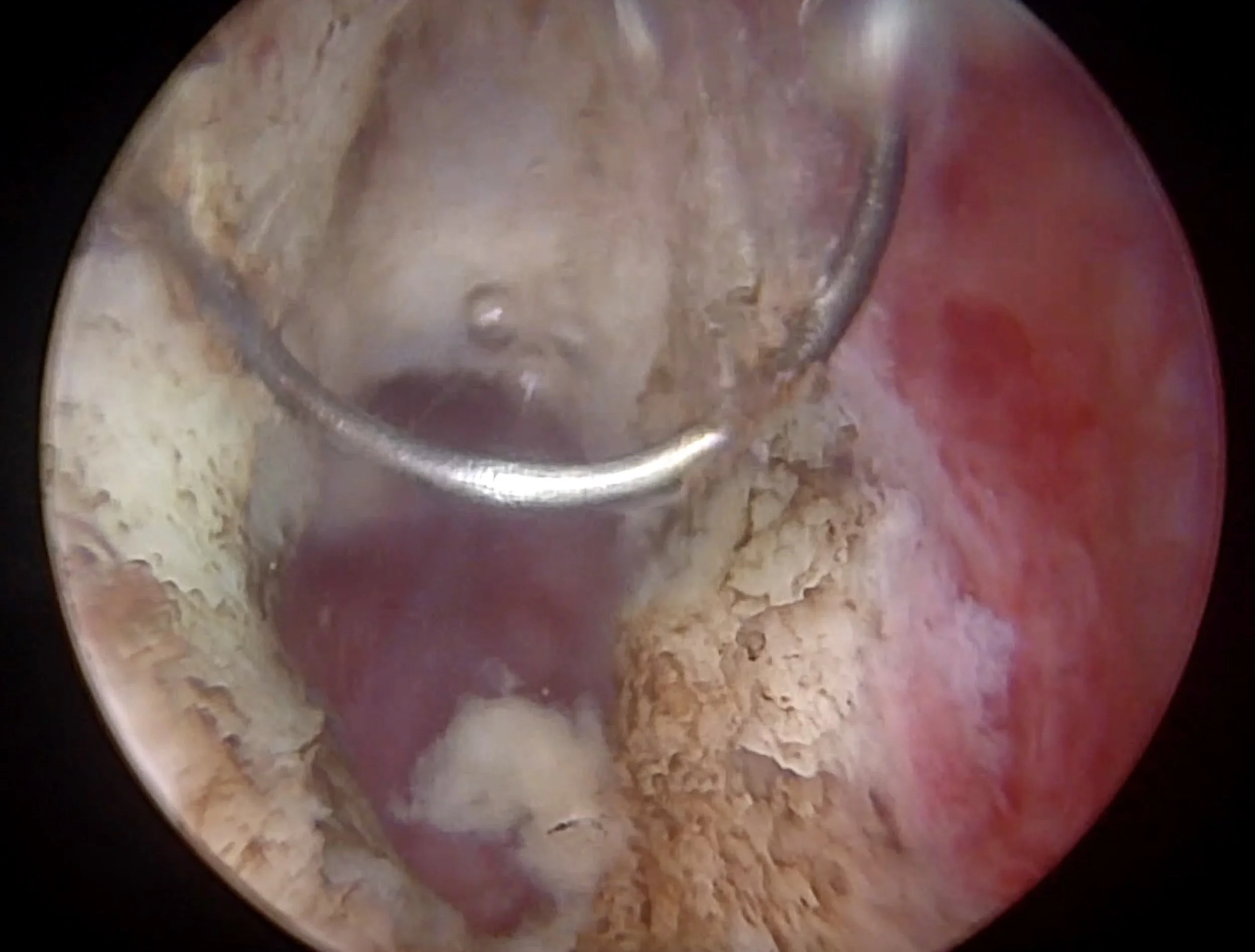
TRUS-guided contrast study with cystoscopy
What is seminal vesiculography?
Seminal vesiculography is a procedure that helps your urologist map the drainage pathway from the seminal vesiclesthrough the ejaculatory ducts into the urethra. It does this by introducing a small amount of contrast dye into the seminal vesicles and observing how it flows.
In your case, this is performed under general anaesthetic with the aid of:
Transrectal ultrasound (TRUS) to guide precise access to the seminal vesicles, and
Cystoscopy (a small camera through the urethra into the bladder) to assess the urethra/prostate region and sometimes confirm dye drainage.
Why might I need this procedure?
Your urologist may recommend seminal vesiculography when they are investigating possible problems with the distal male reproductive tract, such as:
Suspected ejaculatory duct obstruction (EDO)
(which can contribute to low semen volume, infertility, painful ejaculation, or pelvic symptoms in selected cases)Recurrent or persistent blood in semen (haematospermia) in selected situations
Abnormal findings on ultrasound or MRI involving the seminal vesicles/ejaculatory ducts
Clarifying anatomy before/alongside treatment, especially when previous tests have not given a clear answer
What are the benefits?
Depending on your situation, potential benefits include:
Improved understanding of whether the ejaculatory ducts are open or blocked
Identifying patterns that suggest a cause (e.g., poor drainage, obstruction, structural narrowing)
Helping plan the most appropriate next step (observation, medication, further imaging, or procedures such as endoscopic treatment for confirmed obstruction)
Important: This test may not always identify a single clear cause, and results may not always change treatment.
Alternatives
Alternatives depend on your symptoms and previous results, and may include:
TRUS alone
Pelvic MRI (including evaluation of seminal vesicles/ejaculatory ducts)
Seminal vesicle aspiration / washout (aspiration & lavage)
Observation and medical therapy (in selected cases)
Endoscopic evaluation/treatment for confirmed obstruction (in selected cases)
Preparation for surgery
You will receive specific instructions from your clinic. In general:
Fasting
No food for 6 hours before surgery (your anaesthetist may advise differently).
Clear fluids may be allowed up to 2 hours before arrival (follow your instructions).
Medications
Tell your team if you take blood thinners (e.g., aspirin, clopidogrel, warfarin, apixaban, rivaroxaban, dabigatran). You may need a plan to pause/adjust them.
Bring a list of all medications and allergies.
You may be given antibiotics to reduce infection risk.
Bowel preparation
Some practices advise a small enema beforehand to reduce stool in the rectum (TRUS guidance).
Transport
Because you’ll have a general anaesthetic, you must arrange a responsible adult to drive you home and stay with you overnight.
What happens on the day?
Before the procedure
You’ll check in, change into a gown, and meet your surgeon and anaesthetist.
A cannula (drip) is placed.
You will sign consent after discussing the procedure, benefits, and risks.
During the procedure (while you are asleep)
Cystoscopy: A small telescope is gently passed through the urethra to inspect the urethra, prostate channel, and bladder.
TRUS guidance: An ultrasound probe is placed in the rectum to visualise the prostate and seminal vesicles.
Seminal vesiculography: Under TRUS guidance, a fine needle is used to access one or both seminal vesicles and a small amount of contrast is injected. Imaging is used to assess filling and drainage patterns.
In some cases, your surgeon may also take a sample or perform a washout if that is part of your plan (your consent form should reflect this).
Duration
Procedure time varies, but is commonly 30–60 minutes (plus recovery time).
After the procedure
Recovery
You will wake in recovery and be monitored until you are comfortable and stable.
Most patients go home the same day.
What is normal afterwards?
For several days you may notice:
Mild burning when passing urine
Mild pelvic/perineal discomfort or “deep ache”
A small amount of blood in the urine initially
Blood-stained semen for several ejaculations (this can look dramatic but is usually temporary)
Activity
Rest for the remainder of the day.
Light activity the next day is fine.
Avoid strenuous exercise/heavy lifting for 48 hours (or as advised).
Pain relief
Paracetamol is usually enough.
Avoid anti-inflammatory medications if you’ve been advised not to (especially if bleeding risk is a concern).
Sexual activity
You can usually resume sexual activity when comfortable (often after 48 hours), unless your surgeon advises otherwise.
Risks and possible complications
All procedures carry risk. Your individual risk depends on your health, medications, and exact technique.
General anaesthetic risks (uncommon)
Nausea, sore throat, drowsiness
Allergic reaction (rare)
Heart/lung complications (rare; higher risk with significant medical problems)
Procedure-related risks
Infection: urinary infection, prostatitis, seminal vesiculitis; rarely severe infection requiring hospital treatment
Bleeding: blood in urine, rectal bleeding, or blood in semen (usually temporary)
Urinary symptoms: burning, frequency, urgency; rarely urinary retention needing a catheter
Discomfort/pain: pelvic/perineal ache for a few days
Injury to nearby structures (rare): urethral/bladder/prostate irritation from cystoscopy, or rectal irritation from TRUS
Need for further procedures: if results suggest obstruction or other pathology, additional treatment may be recommended
When to seek urgent medical help
Seek urgent care (ED/after-hours) if you experience:
Fever ≥ 38°C, chills, or feel very unwell
Worsening pelvic pain not controlled with simple pain relief
Inability to pass urine
Heavy bleeding in urine (clots) or significant rectal bleeding
Increasing confusion, shortness of breath, chest pain, or severe dizziness
Follow-up and results
Your surgeon will discuss findings with you and explain what they mean for your symptoms or fertility plan. If samples were sent for testing, results may take several days to 1–2 weeks.
Transurethral resection of ejaculatory duct
What is a TURED?
A Transurethral Resection of the Ejaculatory Ducts (TURED) is a minimally invasive endoscopic procedure performed to relieve blockage of the ejaculatory ducts. Obstruction can interfere with the normal flow of semen and may contributed to infertility, painful ejaculation, low semen volume, or recurrent infections.
The procedure is performed through the urethra (the natural urinary passage) and does not involve external incisions.
Preparation for Surgery
Before surgery, you may undergo:
Semen analysis and hormonal blood tests
Ultrasound imaging (e.g. transrectal ultrasound)
Possibly MRI or vasography, depending on your case
In preparation for surgery:
You will be given specific advice about stopping blood-thinning medications prior to surgery
Do not eat or drink for at least 6 hours prior to surgery
Day of Surgery
The procedure is performed under general anaesthesia
A small camera (cystoscope) is passed through the urethra
The opening of the ejaculatory duct is identified and carefully resected to relieve obstruction
The procedure typically takes 30-60min
a temporary urinary catheter will be placed at the end of the procedure
Expect to stay in hospital overnight
The catheter usually removed the following morning
Aftercare and Recovery
In the first few days
Expect mild discomfort when passing urine
Light bleeding in urine and semen is expected to
Activity
avoid heavy lifting, strenuous exercise and sexual activity for 2-4 weeks
Medications
You will be provided specific advice about restarting medications that were withheld for surgery
Follow up
Review appointment usually at 6-8 weeks
Repeat semen analysis may be performed several months after surgery to assess for improvement in semen parameters
Possible risks and complications
While TURED is generally safe, potential risks include:
Common
Blood in urine for a short period, sometimes with small clots
Burning, frequency and urgency when passing urine for a few days
Watery ejaculate (low viscosity) - usually permanent
importantly does not necessarily indicate infertility
Epididymitis/epididymo-orchitis which can cause scrotal pain and swelling and may require antibiotics
Uncommon
Acute urinary retention
Urinary reflux into the ejaculatory ducts/seminal vesicles which is one proposed reason epididymitis can occur after TURED
Urinary tract infection
Recurrence/persistence of obstruction
Rare but important
Retrograde ejaculation - ejaculate flowing backward into the bladder rather than out through the penis
Urinary incontinence
Rectal injury
Urethral stricture/scarring

When to Seek Medical Advice
Contact your doctor or seek urgent care if you experience:
Worsening bleeding
New scrotal pain/swelling
Inability to pass urine
Fever
Any concern about worsening symptoms